
5 Ways Telemedicine is Helping Rural Hospitals & Their Communities
Change has been hard on rural hospitals and their communities. Since 2010, more than 48 rural hospitals have closed and much more are on the brink of the same fate. Patients are seeking higher levels of specialized care from urban hospitals while rural communities are struggling to find top-notch providers willing to reside in remote areas. Lack of resources, provider shortages, and all-time low patient censuses are causing more and more hospitals to consider closing their doors.
But according to a Becker’s Hospital Review article, many believe that virtual health could be the answer to much of the woes rural hospitals are experiencing.
1- Patients are looking for more specialized services
When patients within rural communities contract long-term illnesses that require more extensive testing and monitoring, they’re often forced to spend additional time and resources on traveling to larger hospitals and health systems that are more equipped to provide the care they need. This could include regular check-up appointments with specialty physicians or more in-depth tests that require equipment their rural hospital doesn’t have access to. This can cause a snowball effect by taking away the same patient for general care needs that they can certainly receive from their community hospital.
Rural hospitals have quite a number of options when it comes to providing telemedicine to their patients and all are helpful in their own ways to combat the potential churn of a patient.
Remote specialist consultations can allow a rural hospital to connect with the nearest urban hospital and their physicians for specialized services while still retaining the patient and making their care more convenient and low-cost.
Outsourced diagnostic analysis allows patients to receive diagnostic tests followed by top-notch care depending on the outcome. Patients no longer need to travel for hours just to have an x-ray or specialty lab work performed.
Remote consultations allow doctors to perform routine check-in appointments with patients from home. Not only do they get to skip the long drive to their nearest urban hospital, they can even avoid the short commute to their rural hospital while still seeing their same physician.
Direct-to-consumer telemedicine allows rural hospitals to expand their services to new patients. Patients who don’t typically take the time to see a doctor can now have virtual consultations for urgent care needs without making an appointment, driving to an urgent care, or spending time waiting in the emergency department.
Telemedicine consultations of any kind save time for both the patient and the doctor, leaving room in the physician’s schedule for more appointments with other patients who do require in-person care. Patients in rural areas benefit by removing the barrier of transportation, long drive times and the costs associated with both.
2- Rural hospitals are experiencing provider shortages
There is expected to be an overall shortage of 46,000 to 90,000 physicians by the year 2025 and rural hospitals will feel it. Rural communities are having a hard time attracting physicians who are willing to live in remote areas. Rural communities have about 68 primary care doctors per 100,000 people compared with 84 in urban areas.
Rural hospitals who are experiencing provider shortages can utilize telemedicine platforms that come completely staffed with physicians who are fully trained in providing virtual care, and at a much less expensive rate. Telemedicine platforms who come staffed with 24/7 physician coverage are the perfect solution for small rural hospitals whose emergency departments get overwhelmed with patients not experiencing a true emergency. Patients can access a doctor from home and leave the resident physicians available for truly urgent conditions. Most physicians who staff a telemedicine platform are not primary care physicians, so there is no risk of losing patients to outside providers. In most cases, the physicians can help refer patients back to the hospital for other medical needs.
For hospitals who need an extra benefit to attract physicians from urban areas, according to Dr. Wilbur Hitt in an NEJM career resources article, “telemedicine fosters a collaboration that reduces the feelings of isolation that physicians may experience when they go to practice in a small town,” he said. “With telemedicine, it’s like having one foot in the city but being able to live and practice out in a rural area. It’s also reassuring to know that you’re on the right track with the treatment plan and are staying current.” In addition, it gives rural physicians the opportunity to specialize in something high-tech and innovative that will surely be the way of the future.
3- A high percentage of a rural hospital’s patients receive Medicare
Medicare and the subject of reimbursement often hinder the way a rural hospital can deploy telemedicine to their patients, especially in North Carolina where telemedicine parity doesn’t exist.
Currently, patients in rural areas who are covered by Medicare Part B can be reimbursed for telemedicine services, like office visits and consultations, as long as they are located at one of these places during the telemedicine consultation:
- A doctor’s office
- A hospital
- A critical access hospital
 A rural health clinic
A rural health clinic- A federally qualified health center
- A hospital-based or critical access hospital-based dialysis facility
- A skilled nursing facility
- A community mental health center
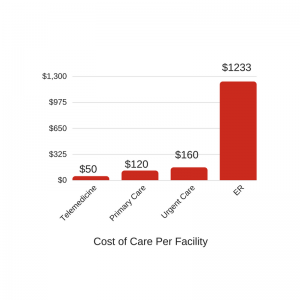
An additional advantage of telemedicine for any patient, including those on Medicare, is that the cost of a visit is much less expensive compared to an urgent care facility or an emergency department visit which often tend to be the first choice for unscheduled care. With most virtual consultations costing less than $50 per visit, patients are able to save on both routine and urgent medical care costs. The savings also applies where insurance isn’t concerned. Non-existant commutes save on the cost of transportation and allow those without means of reliable transit to see a doctor from the comfort of their home.
4- Helping rural hospitals reduce readmissions
Telemedicine is already a proven tool for helping rural hospitals lessen the penalties they receive from value-based reimbursement policies. Rural hospitals who are using telemedicine in addition to implementing care coordination and patient experience improvement strategies are receiving fewer penalties than their urban counterparts.
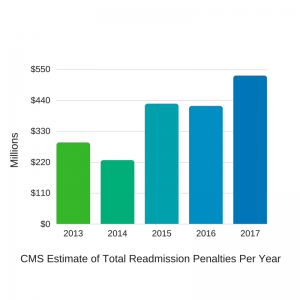 While rural hospitals are already excelling, there is always room for improvement. According to RevCycle Intelligence, rural hospitals still have ways to go under the Hospital Readmissions Reduction Program. 79% of participating rural hospitals faced value-based penalties in 2015 under the program. This year, hospitals will see a 3% maximum rate of penalty and CMS estimates that will total $528 million dollars in penalties across the US.
While rural hospitals are already excelling, there is always room for improvement. According to RevCycle Intelligence, rural hospitals still have ways to go under the Hospital Readmissions Reduction Program. 79% of participating rural hospitals faced value-based penalties in 2015 under the program. This year, hospitals will see a 3% maximum rate of penalty and CMS estimates that will total $528 million dollars in penalties across the US.
A big factor in reducing readmissions is providing better preventive care, this is where telemedicine excels. Remote monitoring allows patients to check in more frequently with their physicians or nurses and also increases the chance that they’ll seek advice when experiencing an unscheduled medical care need before it advances to a more serious condition. By catching a sudden change in status, a patient can be seen by a primary care physician rather than being readmitted to the hospital, thus impacting a hospital’s penalties.
For some patients managing at-home care can be the challenge, especially when dealing with lengthy discharge instructions. When patients aren’t following their discharge instructions correctly, disease symptoms can flare, causing a trip back to the hospital. With remote monitoring via a HIPAA secure video connection, physicians and nurses have the ability to check in on a patient to see if they’re following their discharge instructions correctly and can also administer help remotely for patients who need a little extra hand-holding, this is especially useful for those who do not have at-home care or someone to assist with the fine details.
Prescriptions can also cause problems. Elderly patients may have trouble remembering to fill a prescription, especially when it involves scheduling an additional doctor appointment. By communicating via telemedicine, prescriptions can be refilled during a regular, virtual consultation and can be ready for pick-up at their preferred pharmacy in just a few short hours.
5- Increase patient census & reach the remote and underserved
As mentioned under section #1, direct-to-consumer telemedicine increases a hospital’s reach by attracting patients who otherwise wouldn’t seek care from a rural hospital’s network. Those who live and work in the corners of rural areas have the longest drive time and those who are underserved and do not have reliable transportation usually go without medical care. Even established patients will find value in seeing a doctor from home, greatly increasing their satisfaction of care received.
Telemedicine providers today are able to provide a white-labeled app, meaning they can design both the desktop and mobile interface where patients receive care to use a specific hospital’s brand standards- allowing a patient to seek care from a known and trusted healthcare provider. But, the branding isn’t the most important part. You should also consider how a patient is recognized when using telemedicine provided by your hospital and how their PHI is delivered back to your EHR. While most telemedicine providers can white-label the app, some cannot connect the patient back to your hospital, this creates a fragmented patient record contributing to disparate care coordination.
In addition to being able to tell where a patient is coming from, it also allows the physician providing the virtual care to help the patient determine where they should receive follow-on, in-person care, if necessary. Patients who are linked to one rural hospital can be referred back to that hospital’s network if it makes the most sense.
While rural hospitals are facing increasing challenges, the importance of staying open for the residents of their community is paramount. Telemedicine has proven to be a way forward for many of these hospitals. If you are considering telemedicine and would like to learn more about RelyMD, please reach out.
ADDITIONAL RESOURCES
Case Study
UNC Lenoir Health Care Case Study
Blog Post
Average Wait Times to See a Doctor
