Home / Blog / Reducing Hospital Readmissions with Telemedicine
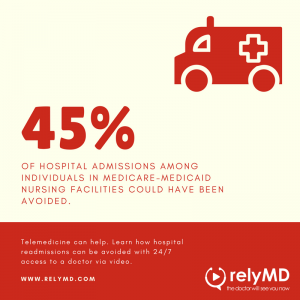 Research completed by CMS found that approximately 45% of hospital admissions among individuals in Medicare-Medicaid nursing facilities could have been avoided. This accounted for $2.6 billion in Medicare expenditures in the year 2005.
Research completed by CMS found that approximately 45% of hospital admissions among individuals in Medicare-Medicaid nursing facilities could have been avoided. This accounted for $2.6 billion in Medicare expenditures in the year 2005.
There are several reasons why SNFs and long-term care facilities should put a large amount of focus on reducing hospital readmissions with telemedicine.
1 – Patients fair better when treated in place: transfers are especially stressful for cognitively impaired residents who are transferred for reasons unbeknownst to them. Hospitalizations often increase the risk of complications, infections, and reduced function upon return to their home facility.
2 – Hand-off communication is lacking: when an elderly resident is transferred off-site, many important health details get lost in translation. Medication errors, wrong-site surgery, and clear communication of symptoms are all things that get misconstrued when being transferred from facility to ambulance to hospital.
3 – Reduced expenditures: keeping residents within their facility and reducing the possibility of empty beds leads nursing facilities to save on Medicare and Medicaid expenditures.
4 – Quality score: as CMS implements their latest initiative to help reduce hospitalizations among nursing home residents, facilities will find that nearly 30% of their overall quality score will be determined by their practice of maintaining an appropriate hospitalization rate.
If it is such a big issue that spans across many different levels, why are facilities still sending out residents who have the potential to avoid the transfer?
1 – Their staff members are not trained to address common medical problems
2 – Physicians aren’t truly available 24/7
3 – They don’t have the tools to communicate changes in resident’s health status to physicians
4 – Fear of litigation
5 – Adult children of residents demand it
Telemedicine offers a way to bridge the gap in care when there isn’t another option to evaluate residents. Actively practicing physicians who are available any time of the day or night can assess a resident’s symptoms via video. With the help of an on-site staff member, these doctors can learn of key vitals and learn of a resident’s normal status compared to the change they’re currently experiencing. The physicians will decide if this is truly an emergency. If it proves to be one of the 45% that are deemed avoidable, the doctor will help the resident’s nurse create an on-site treatment plan that will help keep the resident in-place, but remain on high alert for further changes that would warrant a transfer.
While the focus will remain on reducing hospital readmissions with telemedicine, it’ll also come into play when a transfer is deemed medically necessary. Telemedicine providers that service nursing homes should have a plan in place to help communicate a resident’s health concerns to their receiving hospital. This will help reduce the amount of misinformation an ED doctor receives when administering care to a resident.
It should be noted that the availability of telemedicine will not replace a resident’s primary physician nor should the cost of bringing on this service to all residents equal the amount of an on-call doctor. Telemedicine can be used in place of a primary care physician when they are not available, specifically when they are not on-site or during night shifts. The telemedicine physicians should establish and foster a healthy relationship with a facility’s primary doctor and nursing staff to better coordinate patient hand-offs.
How a Visit Works
1 – A facility nurse has a resident with a medical situation that requires a physician consultation and has the potential for a transfer to the hospital. The facility’s primary doctor is not on site and isn’t available for a phone consultation.
2 – The nurse accesses their telemedicine solution via an iPad or dedicated virtual health computer to connect via video with a physician who is available 24/7.
3 – The nurse and the telemedicine physician review the resident’s health concerns. The nurse will facilitate the visit, helping the physician to see key ailments on the resident’s person while also sharing vitals necessary to appropriately assess the resident’s condition. For things like mental status change, the physician can interact directly with the resident via the video feed.
4 – Once the assessment is complete the physician and nurse will work together to deem whether a transfer is necessary. If a transfer is not necessary, they will establish an in-place treatment plan which includes specific changes to monitor for. If a transfer is necessary, the physician will call the local emergency department to help facilitate a hospital visit and supply all necessary documentation to ensure the transfer is as smooth as possible. The physician is also able to contact the facility’s primary care doctor so they are aware and up-to-date on the status of all patients who have accessed the service.
5 – No matter the outcome, the telemedicine physician will add medical visit notes to the patient’s record to provide clear communication for all parties involved.
Nursing home and long-term care facilities who strategically work at reducing hospital readmissions with telemedicine will see less unnecessary trips to the emergency departments, increased levels of communication among staff members and local hospitals, reduced expenditures, and an optimization of reimbursements. Nursing staff members will be happy with additional support and families will feel confident in the decision for their loved ones to receive specialized care in-place.
Ready to learn how RelyMD can enhance your current benefits package?
Submit the form below and we’ll be in touch soon.
[pardot-form width=”400″ height=”300″ id=”807″ title=”Web Form – Blog – Learn More”]
